Lots of Australians suffers from snoring, while about 2.5 million of Australian adults among those who snore also suffer from obstructive sleep apnea, a common but potentially life-threatening sleep disease. Despite the fact that OSA is quite common, it is frequently misdiagnosed. Pediatric sleep apnea affects even young children. This type of sleep apnea is rather prevalent, although it typically resolves itself without treatment.
However, sleep apnea in adults does not resolve on its own, and therapy is necessary to restore normal breathing during sleep.
Nearly all patients with apnea should try continuous positive airway pressure (CPAP) therapy first. If CPAP stops working after prolonged usage, however, sleep apnea implant surgery may be a possibility. Review the many prerequisites for the implant below before considering the treatment option with a sleep specialist.
Related: The Best Diet for Treating Sleep Apnea
In this article, we will try to address any and all concerns you may have regarding sleep apnea implants by discussing their technique, hazards, eligibility, and efficacy.
What is the function of a sleep apnea implant?
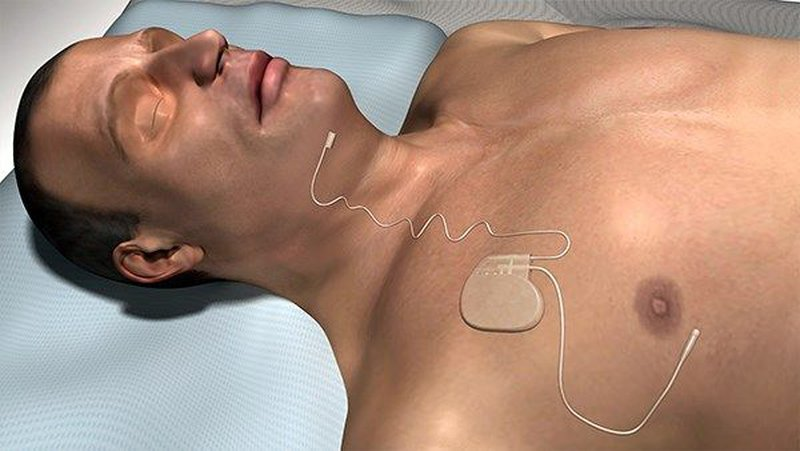
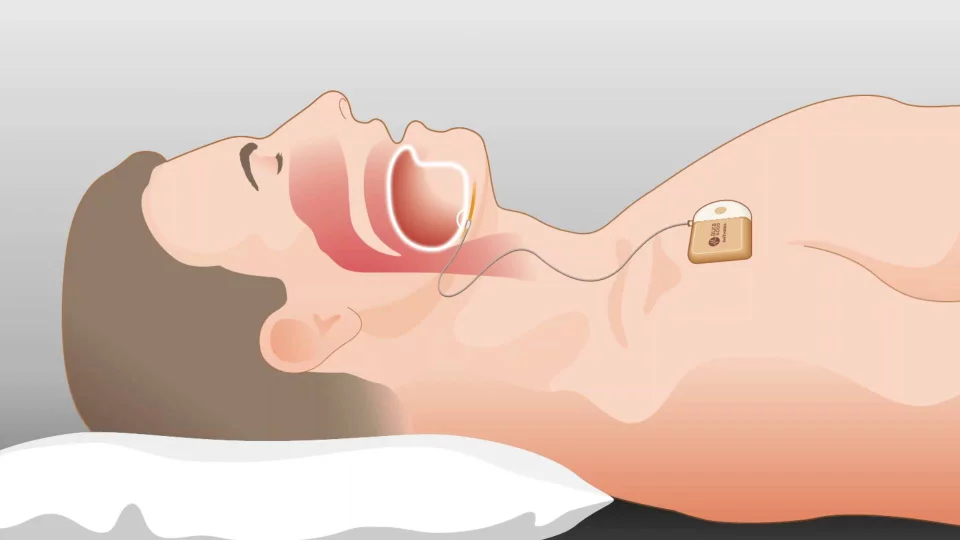
When you have sleep apnea, your airway becomes blocked, and an implant can help by gently repositioning your tongue (hypoglossal nerve stimulation) or stimulating your upper airway (upper airway stimulation treatment). The four primary parts of a sleep apnea implant are:
The remote control may be used to power the device on or off, halt stimulation, or alter the intensity of the stimulation. A chest-implanted breath-monitoring device. When breathing becomes difficult, it sends a signal to the generator, which then sends out electrical impulses to open the airway.
The hypoglossal nerve is stimulated via a cuff of electrodes that is wrapped around the area. These prompt tongue movement by stimulating the nerve that controls it.
The device is surgically implanted in the patient’s upper right chest area, just below the collarbone. Upper airway obstruction is detected by the breathing sensor, which then alerts the stimulation electrode and generator.
The hypoglossal nerve is stimulated mildly, causing movement of the tongue. This will help clear your airway, allowing for easier breathing.
Does implant devices work for getting a good night’s sleep?
However, not everyone with obstructive sleep apnea (OSA) is a candidate for a sleep apnea implant, despite its efficacy in treating OSA symptoms.
In a European Respiratory Journal study, researchers followed 27 patients from three countries who had implanted devices to treat their sleep apnea. The patients’ OSA symptoms, including daytime tiredness, snoring, and quality of life, were monitored throughout the research to see if they improved. Most users logged roughly five nights per week of device time, averaging about five hours each session.
Even though no changes were seen in patients’ BMIs after six months, there was considerable improvement across the board. The number of sleep-related apnea occurrences decreased significantly, while oxygen saturation levels rose. Participants also reported a notable decline in both daily tiredness and overall quality of life. Even the subjects’ sleeping companions said that their snoring had decreased after the surgery.
Though the hazards of a sleep apnea implant are similar to those of any other type of surgical operation.
Who Can Get an Implant for Sleep Apnea?
Similarly, not every patient with sleep apnea will be a suitable candidate for hypoglossal nerve stimulation, even if an implant were available.
You need to be at least 18 years old and have moderate to severe obstructive sleep apnea with an apnea-hypopnea index (AHI) between 15 and 65 to be eligible for surgery. Anyone with a body mass index (BMI) of 32 or more is ineligible for the procedure.
If the following applies to you, you’ll also need to verify that you’ve tried and been unable to endure PAP therapy.
The implant procedure needs to be approved, and that requires more consideration. If you fit any of these descriptions, you should consider seeking help elsewhere if any of the following apply to you:
- You have central sleep apnea, as opposed to obstructive sleep apnea;
- You are pregnant;
- You need frequent MRI scans;
- You have any devices, such as a pacemaker, that might interact with the implant;
- You have a blockage in your upper airway, or a neurological condition that affects the upper airway;
- You have a history of snoring
Which Is Better: CPAP or a Sleep Apnea Implant?
Both treatments aim to increase airflow by opening the airway and lessen the severity of sleep apnea symptoms, but they approach the problem in quite different ways.
Treatment for sleep apnea that involves the use of a machine and a nasal or oral device to keep airways open is called continuous positive airway pressure (CPAP). A constant flow of compressed air from the CPAP machine is piped into your airways via the aforementioned devices. This breeze helps you breathe easier by holding your airways slightly ajar.
The majority of people with sleep apnea can benefit from CPAP therapy, and it is widely available at an affordable price.

Respiratory therapists at sleep clinics help patients who have trouble finding the most comfortable CPAP settings and using them regularly. If CPAP treatment doesn’t work, sleep doctors might try additional methods.
The only way to get an implant for sleep apnea is to go through surgery. This might not be the best choice if you’re hoping to treat your sleep apnea without resorting to surgery. However, a sleep apnea implant may be a good choice for you if you are a good candidate, have tried and failed CPAP, and your insurance will pay the price of the operation which may easily exceed $30,000.
Know When You Need Treatment for Sleep Apnea
The most essential thing is to treat your sleep apnea effectively, regardless of the method you pick. Because OSA’s primary symptoms occur mostly during sleep, many persons with the condition are unaware that they have it. The list of symptoms includes: waking up with a sore or dry throat; loud, chronic snoring that can be heard outside the bedroom; breathing pauses during the night; daytime sleepiness or fatigue; choking or gasping for air while sleeping; feeling tired even after a full night’s sleep; and waking up feeling exhausted.
Schedule an assessment and sleep study as soon as possible if you suspect you have sleep apnea. An accurate assessment of your symptoms or sleep requirements can greatly facilitate your search for an appropriate solution.
Get in touch with the Air Liquide Healthcare right now to get started. Help is at hand if you’ve been deprived of a night’s sleep necessary for your physical and mental well-being.

